Inflammatory Bowel Disease
What is the Difference Between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS)?
IBD and IBS are two illnesses that can affect the gastro- intestinal (GI) tract. Both can cause abdominal pain and changes in bowel movements; however, they are not
the same. While there are many similarities between IBD and IBS, it is important to highlight the differences.
:IBD
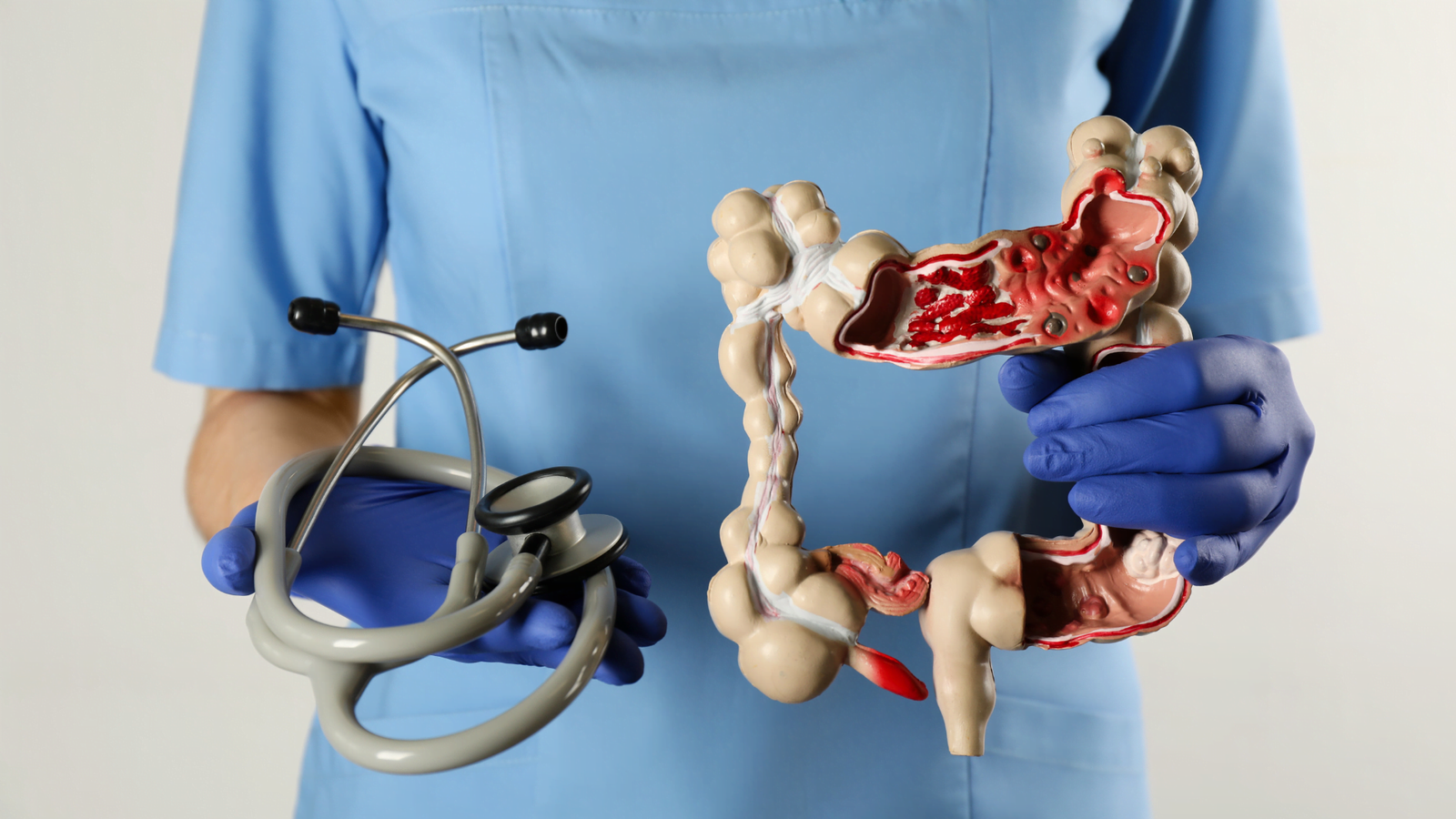
Chronic inflammatory diseases involving the GI tract, including Crohn’s disease and ulcerative colitis.
Immune cells cause inflammation and ulceration in the lining of the intestines, which can lead to frequent and/or urgent bowel movements, abdominal pain, diarrhea, or bleeding.
In IBD, the GI tract is damaged. Symptoms can be different for everyone and depend on the type of IBD and where the inflammation is located in the GI tract.
:IBS
.Functional GI disorder that causes recurrent abdominal pain and changes in bowel movements
.Symptoms may include bloating, constipation, diarrhea, or mixed diarrhea with constipation
.Patients with IBS have these symptoms without damage to the GI tract
.Endoscopy and radiology tests do not show inflammation
Inflammatory Bowel Disease
IBD is a term for chronic inflammation of the gastrointestinal tract. The two most common inflammatory bowel diseases are Crohn’s disease and ulcerative colitis (UC). IBD affects as many as 3.1 million Americans,1,2
most of whom are diagnosed before age 35. There are currently no cures for IBD, but there are treatments to reduce bowel inflammation and control the symptoms of the disease.
Crohn’s disease and UC cause chronic inflammation of the GI tract. Crohn’s disease can affect any part of the GI tract, but frequently affects the end of the small intestine and the beginning of the large intestine (colon). The inflammation in Crohn’s disease can involve the entire bowel wall. UC affects only the large intestine (colon) and the rectum. The inflammation in UC involves only the inner lining of the intestine.
Symptoms
The symptoms of IBD vary from person-to-person, may depend on what part of the bowel is affected by inflammation, and may change over time. Common symptoms for Crohn’s disease and UC include frequent and/or urgent bowel movements, diarrhea, bloody stool, abdominal pain, and cramping.
People with IBD may also report symptoms such as fatigue, lack of appetite, and weight loss. People with IBD may have times of active disease (flare), when symptoms and bowel inflammation are present.
They may also have times of remission, when little or no symptoms are present. When bowel inflammation is reduced by taking an effective medication treatment, flares are less frequent.
Causes
The exact cause of IBD remains unknown. Researchers believe that a combination of factors interact, leading a patient to develop IBD.
Inherited genetic risk-
Environmental risk factors-
Imbalance or changes in the intestinal bacteria (gut microbiome)-
An inappropriate reaction from the immune system-
?Who Gets IBD
As many as 70,000 new cases of IBD are diagnosed in the .United States each year
In Saudi Arabia , the Mean incidences of IBD are increasing in all regions of Saudi Arabia according to Dr. El Mouszan and his group3
Age: IBD can occur at any age, but the median age of diagnosis is 29.5 years for Crohn’s disease and 34.9 years for ulcerative colitis.4
Gender: In general, IBD affects men and women equally-
Diagnostic Procedures
To help confirm a diagnosis of Crohn’s disease or UC, one or more of the following tests and diagnostic procedures may be performed:
- Blood tests: Including red and white blood cells, platelets, and C-reactive protein (CRP)
Tests may be performed to help healthcare pro- viders differentiate IBD from non-IBD. Blood tests can be used to evaluate a patient’s risk of developing disease complications, or to check if and how medications are working in the body.
- Stool tests: Stool tests may check for infection or inflammation (fecal calprotectin) in the GI tract by examining levels of a protein in the stool called fecal calprotectin.
Faecal calprotectin testing can also improve the diagnostic pathway for patients with IBD, ensuring appropriate referral and earlier diagnosis. It was found that multiple algorithms were being used throughout England using cutoffs at 50, 100, 150, 250 microgram/g and it is clear that more evidence is required to determine the most appropriate level.
Cut-offs can only be used as a guide, and irrespective of what cut-off is used a balance between sensitivity and specificity is required.( proposed algorithm which is adopted from National Institute for Health and Care Excellence). 6 can be used to guide the primary health care providers.
The red flags index score (RFS) was recently developedas a clinical tool to predict early diagnosis of Crohn’sdisease. 7 The 8 variables included in the final score are:(1) Nonhealing or complex perianal fistula or abscessor perianal lesions (apart from hemorrhoids); (2)
first‐degree relative with confirmed IBD; (3) weight loss (5% of usual body weight) in the last 3 months; (4)chronic abdominal pain (>3 months); (5) nocturnaldiarrhea; (6) mild fever in the last 3 months; (7) noabdominal pain 30–45 min after meals, predominantlyafter vegetables; (8) no rectal urgency. An RFS ≥8was significantly associated with having Crohn’sdisease compared to IBS and healthy controls with a sensitivity and specificity of 0.94 (95% CI: 0.88–0.99)and 0.94 (95% CI: 0.90–0.97), respectively, and an area under the curve of 0.97 (95% CI: 0.94–0.99). 7
- Endoscopic procedures:
Crohn’s disease and ulcerative colitis:
colonoscopy and Imaging studies help the Gastroenterologist to identify the disease.
IBD Complications
Possible complications of IBD can include:
- Bowel obstruction
- Deep ulcerations
- Extraintestinal manifestations
- Infection
- Malnutrition
Irritable Bowel Syndrome
IBS is a condition that affects the function and behavior of the intestines. Normally, the muscles lining the intestines contract and relax to move food along the digestive tract. In IBS, this pattern is disturbed, resulting in uncomfortable symptoms. In addition, there can be a disturbance in sensation, with heightened sensitivity to normal gas or stool passing through the GI tract. It is important to remember that patients with IBD can also have IBS, but having IBS does not lead to IBD.
Symptoms
Many people experience mild symptoms of IBS, but for some, symptoms can be severe. Symptoms can include cramping, abdominal pain, bloating, gas, mucus in the stool, diarrhea, and/or constipation. Much like IBD, there may be times when symptoms are present and times when little or no symptoms are present. But, unlike IBD, IBS does not cause inflammation, does not cause permanent damage to the GI tract, and does not increase the risk of colorectal cancer.
Causes
The exact cause of IBS is unknown. Potential causes may include sensitivity of the GI tract to gas and bloating, changes in the microbiome (organismsin the gut), or changes in the levels of specific compounds or chemicals within the body, such as serotonin—a chemical in the body that helps regulate mood and social behavior. Although stress does not cause IBS, many people with IBS notice that stress does aggravate their symptoms. Having IBD or a recent GI tract infection (like gastroenteritis) can increase the risk for developing IBS.
Who Gets IBS?
Roughly, prevalence of IBS was 31.8% among Saudi population. 8
- Age: IBS occurs in all age groups, but is most commonly diagnosed in individuals under age 50.
- Gender: IBS is more common in women.
- Family history: Research shows that many people with IBS have a first-degree relative (parent, child, or sibling) with the disorder.
- Infection: Around 40% of people who develop IBS do so after an infection in their digestive system. After the infection clears, the symptoms remain (i.e., post-infectious IBS).
- Psychological history: Some studies indicate that psychological distress, especially anxiety, depres- sion, and childhood trauma, may be risk factors.
Diagnostic Procedures
Diagnosing IBS typically involves a physical exam and medical history. It is important to exclude other GI conditions. The Rome IV criteria defines IBS as recurrent abdominal pain, on average one day
a week in the last three months, associated with at least two of the following:
1) Relation to defecation (discharging feces)
2) Change in frequency of stool
3) Change in the form (appearance) of the stool.
The evaluation may include blood tests, stool samples, endoscopic procedures, or imaging procedures
(like a CT scan or MRI). In patients with IBS, anemia is not apparent, stool calprotectin is normal, and no inflammation is seen on endoscopy or imaging tests.
Complications
IBS can significantly affect quality of life. Research shows that patients with IBS may undergo
more medical testing, as compared with patients without IBS.
Similarities and Differences Between IBD and IBS
References
- Loftus EV, Jr., Shivashankar R, Tremaine WJ, Harmsen WS, Zinsmeiseter AR. Updated Incidence and Prevalence of Crohn’s Disease and Ulcerative Colitis in Olmsted County, Minnesota (1970-2011).
- SurveyDescription, National Health Interview Survey, 2015.Hyattsville, Maryland. 2016.
- El Mouzan, M. I., AlEdreesi, M. H., Hasosah, M. & Assiri, A. A. Regional variation of pediatric inflammatory bowel disease in Saudi Arabia: Results from a multicenter study. World journal of gastroenterology.2020.
https://www.ncbi.nlm.nih.govpubmed/27856364
- Santos MPC, Gomes C & Torres J (2018) Familial and ethnic risk in inflammatory bowel disease. Ann. Gastroenterol. (1):14-23.
- Faecal calprotectin diagnostic tests for inflammatory diseases of the bowel.Nice Guidance 2013.
- Danese S, Fiorino G, Mary JY, Lakatos PL, Moja L, Panes J, et al.Development of Red Flags Index for Early Referral of Adults with Symptoms and Signs Suggestive of Crohn’s Disease: An IOIBD J Crohns Colitis 2015;9:601‐6.
Ibrahim NKR, Battarjee WF, Almehmadi SA. Prevalence and predictors of irritable bowel syndrome among medical students and interns in King Abdulaziz University, Jeddah. The Libyan Journal of Medicine. 2013; 8: 10.3402/ljm.v8i0.21287. doi:10.3402/ljm.v8i0.21287

Dr. Shakir Ali Bakkari,MD
GI consultant and IBD specialist at King Saud medical City -Riyadh